Understanding Chest Infection (Pneumonia): Causes, Symptoms, and Treatment
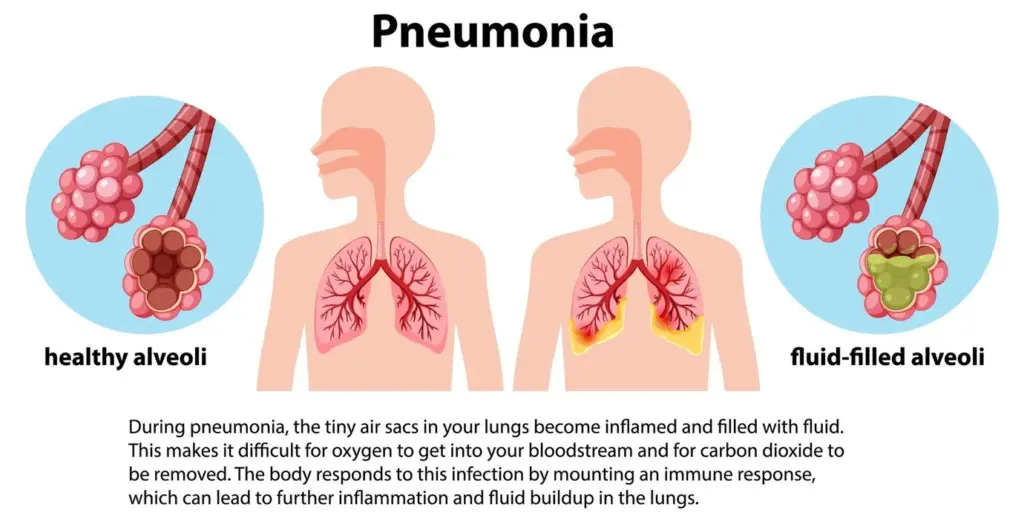
Although they are common, especially during the colder months, chest infections are not all the same. Though some are not serious and may clear up on their own, others, such as pneumonia, can be very severe and potentially life-threatening when not treated. Pneumonia is a serious infection in which the air sacs in one or both lungs become inflamed and fill with fluid or pus. This causes symptoms of cough, fever, and shortness of breath.
Whether you are a strong adult, young child, or senior citizen who is knowledgeable about pneumonia, it can help you get back to feeling healthy. In this post, we’re going to cover pneumonia, including its causes, symptoms, risk factors, and treatments, as well as important preventive strategies.
What is Pneumonia?
Pneumonia is a lung infection involving the alveoli (tiny air sacs), where oxygen exchange takes place. When these sacs are inflamed and fill with fluid, breathing is laborious, as the body fights to take in enough oxygen.
Types of Pneumonia
Numerous infections can cause pneumonia, which can manifest in different ways:
- Bacterial pneumonia – Frequent, it is usually caused by Streptococcus pneumoniae. It can suddenly arrive or appear after a cold or the flu.
- Viral pneumonia – Often due to respiratory viruses such as influenza (the flu) and respiratory syncytial virus (RSV).
- Fungal pneumonia – Uncommon in healthy people but can develop in those with compromised immune systems, including people with HIV or cancer.
Pneumonia is worse than other chest infections like bronchitis (an infection in the airways), because of its severity and the possible dangerous complications.
Causes of Pneumonia
Pneumonia develops when dangerous germs enter the lungs. These can be breathed in from the air or spread from an already infected person.
Primary Causes:
- Bacteria – Streptococcus pneumoniae is the most frequent cause.
- Viruses, such as flu (influenza) and COVID-19.
- Fungi – Such as Pneumocystis jirovecii (in immunocompromised individuals).
How It Spreads:
- Droplets in the air (such as from coughing or sneezing).
- Touching the mouth or nose after coming into contact with unclean surfaces.
Secondary Causes:
- It occurs after a cold or the flu.
- Due to comorbid conditions (COPD, asthma, diabetes, etc.).
Symptoms of Pneumonia
Pneumonia symptoms may be mild or severe, depending on factors such as the type of germ causing the infection, your age, and overall health.
Common Symptoms:
✔ A persistent cough that may produce phlegm (crimson, yellow, or green mucus).
✔ Sharp, stabbing chest discomfort that worsens with coughing or breathing.
✔ Shortness of breath (even when active).
✔ Body aches, a fever, chills, and the shivers.
✔ Fatigue and weakness.
Other Signs:
- Rapid heartbeat.
- Loss of appetite.
- Dizziness (mostly in older individuals).
You should consult with your doctor if you or a loved one experiences these signs.
Risk Factors
Some people are more susceptible to pneumonia, including:
- Older people (over 65).
- Young children (those under 2 years of age).
- Smokers (lung defences damaged).
- Those with underlying health conditions (such as asthma or heart disease).
- Immunocompromised individuals (transplant recipients, high-dose corticosteroids, etc.).
Hospitalised patients, particularly those who are mechanically ventilated (increased risk of hospital-acquired pneumonia, HAP).
Diagnosis of Pneumonia
- Physical exam – Checking for crackles or wheezing in your lungs.
- Chest X-ray or CT scan – To demonstrate lung inflammation.
- Blood tests – They look for markers of infection (e.g., white blood cell count).
- Sputum test – Microbiological examination to identify the pathogens.
The right treatment happens when the diagnosis is made early.
Treatment Options
Medical Treatments:
- Antibiotics (to treat bacterial pneumonia).
- Antivirals (if it’s pneumonia from viruses, like oseltamivir for flu).
- Antifungals (for fungal infections).
Supportive Care:
- Fever reducers (such as paracetamol).
- Oxygen therapy (if blood oxygen levels are low).
- Hospitalisation (in severe cases, particularly for high-risk patients).
Self-Care at Home:
- Rest to help the body heal.
- Stay hydrated to help loosen mucus.
- Do not smoke and avoid air pollution.
Recovery and Aftercare
Recovery time varies:
- 1–2 weeks for mild cases.
- Weeks to months for severe pneumonia.
Tips for Faster Healing:
✔ Complete all medications as directed (even if you begin to feel better).
✔ Reintroduce activities slowly (do not overdo it).
✔ Schedule follow-up check-ups to track recovery.
Prevention of Pneumonia
Vaccinations:
- Pneumococcal vaccine (protects against Streptococcus pneumoniae).
- Flu vaccine (because flu can trigger pneumonia).
Lifestyle Measures:
✔ Wash your hands frequently to keep germs at bay.
✔ Avoid close contact with sick people.
✔ Stop smoking to protect your lungs.
We provide vaccination and health advice at Chase Lodge Hospital to help keep you safe from pneumonia.
When to See a Doctor
Get emergency medical help if you have:
⚠ Very high fever (38°C and above) that is not improving.
⚠ Severe difficulty breathing or bluish lips/nails (a sign of low oxygen).
⚠ Confusion, chest pains, or coughing up blood.
Conclusion
Pneumonia is a severe but treatable infection. If you recognise the symptoms and get medical attention early, you can avoid complications and help speed up recovery. At Chase Lodge Hospital, we offer the very best in diagnosis, treatment, and ongoing care for you and your family.
If you believe that you have pneumonia or if you’d like to learn more about vaccinations, schedule your appointment online with our physicians today. Keep informed, stay safe!