Understanding Urine Incontinence – Causes, Management & Treatment
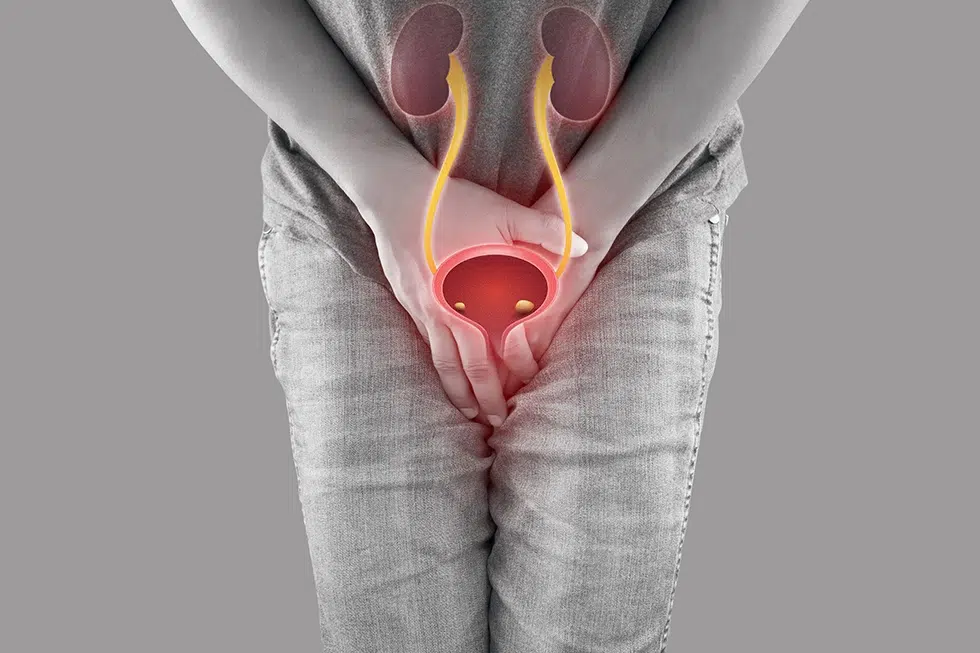
Urine incontinence (also called as bladder leakage) can be described as the involuntary emission of urine. Though it may feel horribly embarrassing, this is much more common than many appreciate, affecting millions of people in the UK. The problem can affect self-esteem, emotions, and daily life. Urine incontinence is an equal-opportunity condition, one that can impact men and women alike, though the causes and risk factors tend to differ by sex. Fortunately, it’s a treatable condition with lots of treatment and support options to choose from. In this post, we will go over the causes, types, and treatments, from men’s urine incontinence pads to medication.
What is Urine Incontinence?
Urine incontinence is the inability to control the release of urine, resulting in involuntary loss of urine. This could be occasional dribbles between coughs and sneezes or an uncontrollable urge without warning leading to accidents.
Spasms are typically not harmful but if you’re experiencing leakage during activity, you may have an underlying problem that needs attention from your primary care provider. Difference Between Triggers: Some women will have a leakage with laughing, coughing, or lifting heavy objects, while others may feel a strong urge to go to the bathroom and then are unable to make it there in time. Understanding the type and frequency of incontinence is the first step to the right solution.
Urine Incontinence Causes
Incontinence of urine has a multitude of causes, and your incontinence may be related to which type you’re experiencing:
- Stress Incontinence: This happens when physical activity (for example coughing, sneezing, or heavy lifting) puts a strain on the bladder which causes leakage. It is often the result of weakened pelvic floor muscles, which can be caused by childbirth, surgery, or ageing.
- Urge Incontinence: The type of incontinence where you get a strong urge to pee but can’t make it to the toilet in time, is typically associated with an overachieving bladder. UTI (urinary tract infection), bladder disorder such as inflammation, neurological conditions such as Parkinson’s or multiple sclerosis are common culprits.
- Overflow Incontinence: This occurs when the bladder does not empty all the way, leading to overflow. It can be because of a blockage (like an enlarged prostate in men), nerve damage, or chronic constipation.
- Functional Incontinence: This type of incontinence is not a result of problems with the bladder itself, but instead when the body or brain (like with arthritis or dementia) makes it difficult or impossible to get to the toilet in time.
- Mixed Incontinence: A mixture of stress and urge, this type is very common among women.
Risk factors include old age, obesity, and underlying health conditions such as diabetes, as well as lifestyle factors like smoking or inactivity.
Types of Urine Incontinence
There are five types of incontinence that are defined:
- Stress Incontinence: The loss of small amounts of urine with physical activities, such as coughing or exercising, that put pressure on the bladder.
- Urge Incontinence: Sudden and strong urges to urinate accompanied by leakage of urine.
- Overflow Incontinence: Dribble all the time not fully emptying the bladder.
- Functional incontinence: Not reaching the bathroom in time because of a physical or cognitive impairment.
- Mixed Incontinence: A blend, usually of stress and urge incontinence.
Every entity consists of its own management and treatment strategy.
Diagnosis of Urine Incontinence
A complete review of symptoms and medical history will be conducted, and if necessary, physical exams will be performed:
- Pelvic or prostate exam to evaluate for tone or abnormalities.
- A urinalysis to eliminate the possibility of infections or blood in the urine.
- Bladder scans and urodynamic testing to assess pressure and functionality of the bladder.
- On occasion, cystoscopy (passage of a thin tube into the bladder) can be carried out.
These evaluations aid in identifying the cause and a rational treatment approach.
Management & Treatment Options
Lifestyle and Behavioral Modifications
Most people benefit from non-medical approaches, particularly in the early days:
- Kegel exercises to strengthen the muscles in your pelvic area and help you control your bladder.
- Bladder training, in which people practice scheduled toilet visits and delayed urination, is one way to establish better control.
- Fluid and diet management — minimising bladder irritation by decreasing caffeine, alcohol, and spicy foods.
- Weight loss can reduce pressure on the bladder and the pelvic floor.
Male Urinary Incontinence Pads and Products
For men who are leaking, there are numerous discreet options:
- Gender-specific pads designed for men will give you confidence and protection for the entire day.
- Protective underwear, bed pads, and urine collectors are helpful additions.
- The incontinence products support you in everyday life – including the joy of life!
Urine Incontinence Drugs
Depending on the type of incontinence, several prescription drugs can help:
- Anticholinergics (such as oxybutynin or tolterodine) relax bladder muscles to help avoid urgency.
- Beta-3 agonists (for example, mirabegron) are used to manage bladder contractions.
- Alpha-blockers (such as tamsulosin) are often given to men who have urinary problems linked to prostate problems.
- Local oestrogen creams might be beneficial for postmenopausal women with urogenital atrophy.
All medication should be taken under the care of a physician.
Medical Procedures
Treatments for Incontinence In cases of stubborn or severe incontinence, the following interventions may be used:
- Bulking agent injections to aid in sealing the bladder neck closure.
- Nerve stimulation treatments such as PTNS (Percutaneous Tibial Nerve Stimulation) for overactive bladder.
- For more difficult cases, surgical interventions, such as sling operations or implantation of artificial sphincters can be performed.
These choices are generally considered when conservative approaches have failed.
When to Seek Medical Help
Here’s when to see a health care provider:
- The incontinence affects your quality of life, sexual relationship, or emotional well-being.
- You see blood in your urine or feel pelvic pain.
- Symptoms get worse after self-care or over-the-counter treatments.
Early treatment is more successful and can prevent complications down the line.
Prevention Tips
Here are a few simple yet effective ways to mitigate and prevent symptoms:
- Do pelvic floor exercises regularly and even before symptoms start.
- Avoid bladder irritants, such as caffeine, alcohol, and spicy foods.
- Control comorbidities such as diabetes and chronic constipation.
- Keep active and adopt a healthy weight to help reduce pressure on your bladder.
Conclusion
Incontinence is a treatable condition and there are many treatment and lifestyle options available. Whether it’s from stress-related leakage or an overactive bladder, the cure has to match the cause. If you’re worried about symptoms, by all means go ahead and seek professional advice. Incontinence doesn’t have to impact your quality of life with the proper care.
For personalised help, treatment, and support, consult your GP or visit the NHS website.
Chase Lodge Hospital – delivering compassionate, expert care for your urological health.