Understanding Peptic Ulcers (Stomach or Duodenal Ulcers)

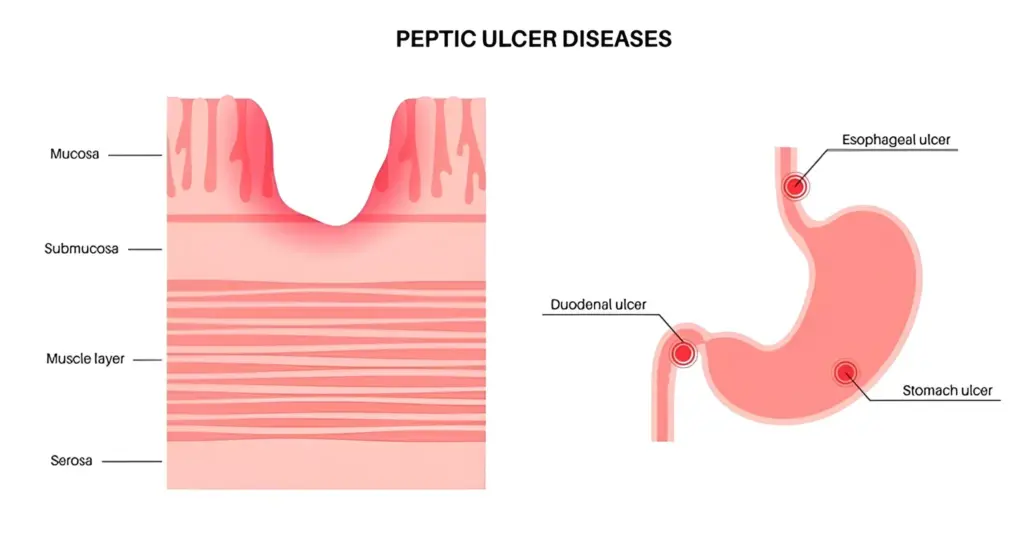
Gastric ulcers, or open sores on the inside lining of the stomach, and duodenal ulcers, or open sores on the upper portion of the small intestine, are peptic ulcers.They happen when the natural lining that protects the digestive tract becomes weakened, and eats away at the delicate tissue underneath thanks to stomach acid.
A burning or gnawing pain in the abdomen is one of the most prevalent complaints of a peptic ulcer, and it usually happens after meals or in the early hours of the morning. Others may feel bloated, nauseous, or too full even after consuming just a small amount of food. Although having peptic ulcers means that it is often necessary to treat them, they may become more severe if they are not managed, in some cases causing internal bleeding, a hole in the wall of the stomach (perforation) or a blockage in the stomach or nearby area of the digestive system.
At Chase Lodge Hospital, that’s what we’re here for. Our seasoned team provides concise diagnosis and customised treatment plans to assist you on the road to recovery and health for the future.
What Causes Peptic Ulcers?
Peptic ulcers occur when there is an acid imbalance between the acid that your stomach produces and the protective lining of your stomach. There are several key causes:
- H. pylori infection: This is the bacterial infection that causes peptic ulcers the most frequently. It renders the stomach more vulnerable to acid by breaking down the protective lining on its walls.
- Overuse of NSAID pain relievers: Ibuprofen, aspirin, or naproxen that’s used regularly can irritate the stomach lining and cause ulcers.
These are:
- Consuming too much alcohol – it can increase acid production and damage the stomach’s lining.
- Smoking – smoking slows the healing process and also increases the chance of ulcers coming back.
- Zollinger-Ellison syndrome – a rare condition that makes the stomach produce too much acid.
|
Myth buster: Stress and spicy food may worsen ulcer symptoms, but they don’t directly cause ulcers. It’s infections and long-term use of NSAIDs that are the main culprits. |
Recognising the Symptoms
Peptic ulcer symptoms can range from person to person, and may include:
- A gnawing, burning or aching pain in the abdomen – typically relieved by having a snack or taking an antacid.
- Feeling bloated or nauseous.
- Vomiting or heartburn.
More serious symptoms to look out for:
- Dark or black-coloured stools – which might suggest bleeding.
- Sudden severe abdominal pain – this could be due to a perforated ulcer.
- Weight loss (that you can’t explain) – and might indicate something worse.
It’s a good idea to seek medical attention if any of these symptoms sound familiar.
How Is a Peptic Ulcer Diagnosed?
If your doctor thinks you have a peptic ulcer, they will order one or more of the following tests:
- H. pylori test – This can be accomplished through blood tests, stool tests or by taking a breath test to see if you have the bacteria in your stomach.
- Endoscopy – To see the stomach and duodenum up close, a flexible camera is placed through the mouth.
- Barium swallow X-ray – Not as commonly done now, but can be done. You swallow a chalky liquid to help ulcers appear on X-rays.
Treatment Options
Simple changes in lifestyle, along with medication, can help alleviate most ulcers.
Medications may include:
- Proton pump inhibitors (PPIs) –Reduce stomach acid production and aid in the healing of your ulcer (e.g. omeprazole, lansoprazole).
- Antibiotics – If you test positive for H. pylori, you’ll require a short course of antibiotics to clear the infection.
- H2 blockers – These work to reduce the amount of acid but are not as frequently used today.
Lifestyle counselling to aid in the healing process:
- Avoid NSAIDs if possible – see your GP for alternatives.
- Quit smoking and cut back on alcohol, if either of those is a live issue.
- Eat small, balanced meals to help aid digestion and prevent irritation.
Is Surgery Ever Needed?
Surgery is necessary in the following rare instances:
- An ulcer is bleeding and not stopping.
- There has been a perforation (a hole in the stomach or bowel).
- Medication is not working well.
What Will Happen If Ulcers Are Not Treated?
If ulcers are not treated, they may cause major side effects such as:
- Internal bleeding – can result in anaemia or a medical emergency.
- Perforation – indicating that a hole has developed, which can cause a serious infection.
- Gastric outlet obstruction – scar tissue may block the passage of food out of the stomach, leading to vomiting and weight loss.
How Can You Prevent Them?
To prevent a new or recurrent ulcer:
- Avoid or minimise NSAID use – and always take them with food.
- Stop smoking and drink in moderation.
- Get treated if you test positive for H. pylori.
Avoiding highly spicy, oily, or acidic foods might help ease unpleasant symptoms, even if diet does not cause ulcers.
Conclusion
Peptic ulcers are both common and curable. With proper medical care and modest lifestyle alterations, most people return to full health. The trick is to be aware of the warning indicators. If the pain, or any of the symptoms, is something that has been bothering you, please don’t wait – talk to someone.
At Chase Lodge Hospital, our experienced specialists are committed to guiding you through each stage of the process and providing the very best care for everyone’s digestive health problems.
Need Help?
If you suspect you could have an ulcer, contact your GP or one of our gastroenterology experts. Early diagnosis and treatment can help you get better faster and can save you from more serious complications.
More reading: For more information, see the NHS guide to stomach ulcers.