Understanding Meningitis: Causes, Symptoms, and Treatment
Meningitis is a serious condition that needs immediate medical attention. It is brought on by inflammation of the meninges, which are membranes that coat the brain and spinal cord. While some cases are mild and go away without treatment, others can be life-threatening and need immediate medical care.
Meningitis can develop rapidly, and recognising the signs can save lives. Regardless of whether they are caused by viruses, bacteria, or other implied causes, the condition affects all age groups, from newborns to older adults.
In this blog, we cover the various forms of meningitis, what causes them, their symptoms, and their treatments. We’ll also talk about how to prevent the condition and what to expect during recovery.
What is Meningitis?
Meningitis happens when the meninges, the thin tissue covering the brain and spinal cord, are inflamed. These membranes are a key structure that acts to shield the central nervous system from both infections and injuries. If they become inflamed because of infection or another reason, they can press on vital structures, resulting in life-threatening complications.
This condition may be caused by different pathogens such as viruses, bacteria, fungi, or parasites. Meningitis can occasionally result from non-infectious causes, such as autoimmune diseases and specific medications.
Types of Meningitis
Viral Meningitis
Compared to bacterial meningitis, the most prevalent kind, viral meningitis is frequently less severe. It is often caused by enteroviruses but can also be ascribed to herpes, mumps, or flu viruses.
Key facts:
- Transmission is by droplet (aerosol) or fomites.
- Symptoms can mimic the flu, but with severe headache and neck stiffness.
- In most cases, it clears up without treatment, but the recovery process may take weeks.
Bacterial Meningitis
This variant is less common but much more dangerous. Its consequences, if left untreated, can be brain damage, hearing loss, or death.
Common bacteria responsible:
- Meningococcal (Neisseria meningitidis) – Causes a sudden onset of disease and can sometimes result in sepsis (blood poisoning).
- Pneumococcal (Streptococcus pneumoniae) – It occurs more frequently in babies and the elderly.
- Group B Streptococcus – It commonly occurs in newborns.
Why it’s dangerous:
- Symptoms can escalate rapidly, within hours.
- Need to be hospitalised immediately with IV antibiotics.
Other Types of Meningitis
- Fungal meningitis is rare and usually occurs in people with compromised immune systems.
- Parasitic meningitis – Very rare, but those are the worst (e.g., Naegleria fowleri or the “brain-eating amoeba”).
- Non-infectious meningitis – Caused by autoimmune disorders, cancer treatments, or some medications.
Causes and Risk Factors
How is Meningitis Spread?
- Close personal contact (such as kissing or touching).
- Common things (for example, utensils, a toothbrush).
- Mum to baby during delivery (Group B Strep).
Who is Most at Risk?
- Infants and young children, whose immune systems are still developing.
- Teenagers and young adults (as a result of close living, such as in university halls).
- Older people and individuals with compromised immune systems (such as HIV patients, chemotherapy patients).
- Unvaccinated individuals (for example, those who have missed routine NHS immunisations).
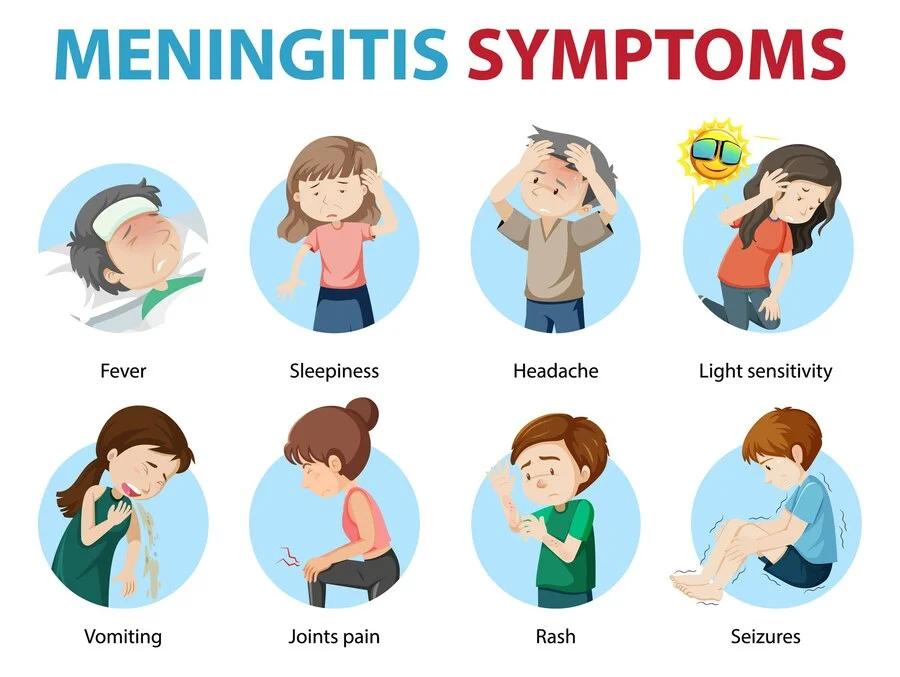
Signs and Symptoms
In Adults and Older Children
- Sudden high fever
- Very extreme headache (the worst ever experienced).
- Neck stiffness (cannot touch chin to chest)
- Nausea and vomiting
- Feeling sensitive to light (photophobia)
- Feeling confused or having trouble focusing
In Babies and Young Children
- High-pitched crying
- Bulging in the fontanelle (soft spot) of an infant’s head
- Unusual drowsiness or fussiness
- Refusal to feed
- Stiff body or floppiness
When to Seek Emergency Help
Meningitis can also worsen quickly. Go to A&E or call 999 straight away if you or someone has:
- An abrupt, high fever along with a very severe headache
- Neck stiffness and confusion
- A non-blanching rash (a sign of meningococcal sepsis)
- Fits or passing out
Diagnosis
- Physical examination – Look for rigidity of the neck, rashes, and signs of neurological problems.
- Blood test – Infection markers and the presence of bacteria/viruses can be detected.
- Lumbar puncture (spinal tap) – Testing cerebrospinal fluid for infectious agents.
- Imaging scans (CT / MRI) – These are used to eliminate brain swelling or abscesses.
Treatment Options
Bacterial Meningitis
- Hospital care is immediate – IV antibiotics and steroids are given to bring down the inflammation.
- Quarantine may be required in case of infection.
Viral Meningitis
- Rest, fluids, and analgesics (e.g., paracetamol) are usually curative for most cases.
- In the severest cases (e.g., herpes-related), antiviral agents may be required.
Fungal or Parasitic Meningitis
- It needs long-term antifungal or antiparasitic therapy.
Complications of Meningitis
In some patients, there can be prolonged symptoms even after one recovers, including:
- Hearing loss
- Problems remembering and concentrating
- Seizures or epilepsy
- Motor skill impairments
- Children who have had meningitis may require continued developmental support.
Prevention
Vaccinations (Key in the UK)
- MenB vaccine – given to babies at 8 weeks, 16 weeks, and 1 year.
- MenACWY vaccine – offered to teenagers and university freshers.
- Pneumococcal vaccine (PCV) – Prevents Streptococcus pneumoniae.
- Hib vaccine – Protects against Haemophilus influenzae type b.
Healthy Practices
- To reduce the chance of illness, wash your hands frequently.
- Don’t share drinks, utensils, or toothbrushes.
- Keep on top of NHS-recommended jabs.
Living After Meningitis
Recovery varies—some people bounce back quickly, while others face long-term challenges. Follow-up care is crucial, especially for children, to monitor hearing, vision, and cognitive development.
Conclusion
Meningitis is a medical emergency. Recognising the symptoms early and acting fast can mean the difference between life and death. Vaccination remains the best defence, so ensure you and your family are protected.
If you suspect meningitis, do not wait—seek emergency care immediately. For more information or vaccination advice, contact Chase Lodge Hospital.
Stay informed, stay protected.