Understanding Kidney Failure: Causes, Symptoms, and Life with Treatment
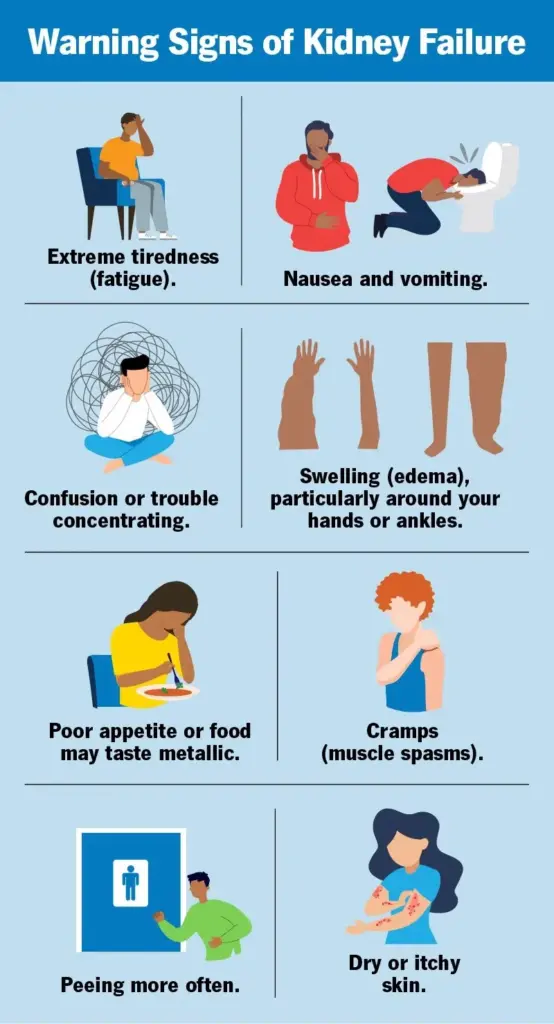 Image Source: my.clevelandclinic.org
Image Source: my.clevelandclinic.org
The two tiny, bean-shaped kidneys help maintain the cleanliness and well-being of your body. They filter waste, maintain fluid balance, control blood pressure, and make hormones we need to build red blood cells and promote bone health. But when they begin to fail to function properly, it can cause kidney failure — a life-threatening condition that requires immediate medical intervention.
Your kidneys stop working well enough for you to survive when they lose their ability to function, resulting in a dangerous buildup of waste and fluids in your body. With early detection and management, quality of life can be greatly sustained with dialysis, transplantation, or lifestyle changes.
On the blog topic of kidney failure, let’s dive into how kidney failure arises, what it feels like, how it gets diagnosed, and what you can do about it, along with tips for living life well with this condition.
What is Kidney Failure?
The Role of Kidneys in the Body
Your kidneys do a lot of important work:
- Filtering the blood – Clearing the body of harmful compounds, such as toxins, salts, and waste products, after metabolism.
- Fluids and Electrolytes – Maintaining sodium, potassium, and water.
- Producing hormones, such as renin (which aids in blood pressure regulation) and erythropoietin (which promotes the formation of red blood cells).
What Happens When Kidneys Fail?
Toxic chemicals accumulate in the body after renal failure, leading to:
- Fluid retention: You may experience facial, ankle, or leg oedema.
- Electrolyte disturbance – Which can disrupt the heart and muscles.
- Anaemia – As a result of decreased production of erythropoietin.
- Hypertension – Gradual decline in kidney function over time.
Types of Kidney Failure
Acute Kidney Injury (AKI)
- Abrupt onset, because of serious dehydration, infections, or as a side effect of medication.
- May reverse; treat rapidly.
Chronic Kidney Disease (CKD)
- Starts slowly, sometimes evolving over the years.
- Permanent in advanced stages, and must be controlled long-term.
- Top causes: Diabetes, high blood pressure, polycystic kidney disease.
Common Causes and Risk Factors
Medical Conditions
- Diabetes – Elevated blood sugar level is the chief culprit, resulting in damage to the kidney blood vessels.
- High blood pressure – Higher pressure is detrimental to kidney tissues.
- Glomerulonephritis – Inflammation of the glomeruli in the kidneys.
- Hereditary conditions, such as polycystic kidney disease.
Lifestyle and Medicine Risks
- Excessive use of painkillers (NSAIDs such as ibuprofen).
- Smoking and too much alcohol reduce the flow of blood through the kidneys.
- Unhealthy eating habits – Salty and processed food, and less water intake.
Signs and Symptoms of Kidney Failure
Early Warning Signs
- Fatigue: A consequence of both anaemia and the buildup of toxins.
- Oedema, or swelling, can occur in the legs, feet, and around the eyes.
- Urinary symptoms – Dark, foamy, or frequent urination.
Advanced Symptoms
- Vomiting and nausea – Due to the retention of waste.
- Cramps in muscles – Can be because of loss of electrolytes.
- Breathlessness – Accumulation of fluid in the lungs.
- Delirium – Poisons that confuse the brain.
Diagnosis of Kidney Failure
Blood Tests
- Creatinine & Blood Urea Nitrogen (BUN) – Higher values or increased levels in kidney dysfunction.
- The estimated glomerular filtration rate (eGFR) is a measure of the kidneys’ filtering efficiency.
Urine Tests
- Urine protein: An excessive amount of protein in the urine indicates renal impairment.
- Haematuria – The presence of blood in urine indicates infection or disease.
Imaging & Biopsy
- Ultrasound or CT scan – Looks for structural anomalies.
- Biopsy of the kidney – It may be performed in some instances to confirm the reason for failure.
Treatment Options for Kidney Failure
Dialysis
- Haemodialysis – Blood is cleaned using a machine 3-4 times a week.
- Peritoneal dialysis – This method uses the lining of the abdomen to filter blood at home.
Kidney Transplant
- Best long-term solution, but a donor match is needed.
- Immunosuppressants forever – To prevent rejection of the organ.
Palliative Care
- For patients who choose non-dialysis management, comfort is the primary goal.
Lifestyle Changes and Management
Dietary Adjustments
- Low in sodium, potassium, and phosphorus – For the reduction of kidney burden.
- Controlled protein intake – Producing less waste.
- Fluid restriction – Intended to medically manage severe swelling.
Medications & Mental Health
- Blood pressure medications — ACE inhibitors or ARBs.
- Erythropoietin injections – To control anaemia.
- Counselling & Support groups – Living with a chronic illness.
Living with Kidney Failure
- Routine check-ups – Keeping track of kidney function and making changes as needed to treatment.
- Keeping active – Mild activity such as walking or yoga.
- Support systems – Family, friends, and patient communities.
Prevention Tips
- Manage blood pressure and sugar – To avoid CKD.
- Drink plenty of water – Good for flushing toxins from the kidneys.
- Be careful with NSAIDs – Avoid excessive use.
- Screen regularly – Especially for diabetics or hypertensives.
Conclusion
Kidney failure is a serious condition that can be treated, but it is not a pleasant experience. If detected early, promptly treated, and lifestyle changes are made, outcomes can be substantially enhanced. If you or a loved one has symptoms, be sure to seek medical advice promptly.
At Chase Lodge Hospital, our nephrologists treat you as an individual and give you support to lead a normal life with kidney disease. Schedule a consultation today and get on the road to improved kidney health.