Understanding Ear Infections (Otitis Media): Causes, Symptoms, and Treatments
Ear infections or Otitis Media (OM) are a prevalent, usually painful infection of the middle ear, common in young children and adults. Ear infections, whether they be sharp and sudden or persistent and dull, can interrupt daily activity and can be a more serious issue if left untreated.
By the time they are ten years old, almost one in four youngsters in the UK will have ear infections. But adults are not immune, especially those who have allergies, sinus problems, or a weakened immune system. This guide will cover Otitis Media causes, symptoms, and treatment, teaching you how to spot when to get medical help as well as protecting yourself from it happening again.
What is Otitis Media?
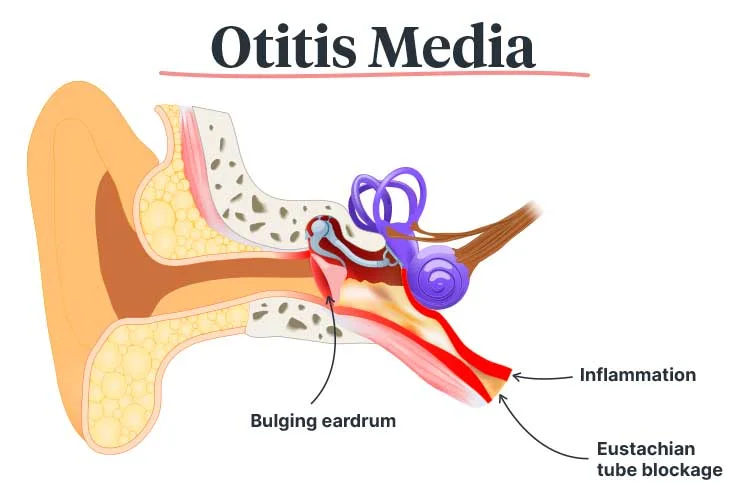
Otitis Media is a condition of infection or inflammation of the middle ear – the air-filled space behind the eardrum. This is the area of those tiny vibrating bones that are so important to hearing, so if infections are recurring or become chronic in this area, it’s of increased concern.
Types of Otitis Media
- Acute Otitis Media (AOM) – An infection of the ear that is characterised by pain, fever, and, in some cases, discharge of fluid. It usually clears up within a few days or by taking antibiotics.
- Chronic Otitis Media (COM) – A long-standing or recurring infection that can cause constant or chronic fluid in the middle ear and may include a hole in the eardrum.
Appreciating these differences makes choosing the correct treatment more possible.
Causes of Ear Infections
Ear infections typically arise from a confluence of factors:
Infections Caused by Bacteria and Viruses
- The majority are triggered by bacteria (such as Streptococcus pneumoniae) or viruses (such as the cold or flu virus). When respiratory infections ascend to the ear, they cause inflammation and fluid.
Allergies and Sinus Infections
- Allergies or sinus congestion can clog the Eustachian tube, which is a skinny passageway that connects the middle ear to the throat, and can cause fluid to become stuck and infected.
Eustachian Tube Dysfunction
- Drainage is more difficult in youngsters since the tube is shorter and more horizontal. The risk increases if conduits become blocked by colds, allergies, or enlarged adenoids.
Environmental and Morphological Parameters
- Secondhand smoke exposure
- Elevated bottle feeding (one option – lying down) (increased fluid reflux into the ear)
- Craniofacial anomalies (e.g., cleft palate, Down’s syndrome)
Common Symptoms to Watch For
In Children:
- Pulling or rubbing the child’s ears indicates that they are uncomfortable.
- Irritability, insomnia, or changes in eating habits
- Fever (often above 38°C)
- Fluid drainage from the ear
In Adults:
- Ear pain or a feeling that the ear is blocked up
- Hearing loss or impairment for some time
- Dizziness or balance issues
- Persistent headaches
Since children may not always verbalise their discomfort, observing behavioural changes is key.
How is an Ear Infection Diagnosed?
Physical Examination
With an otoscope, a physician can examine the eardrum to look for redness, swelling, or fluid behind the eardrum.
Assessment of Fluid Buildup
- Pneumatic otoscopy assesses eardrum mobility.
- Tympanometry is an evaluation of middle ear pressure.
When to See a Doctor
- Symptoms for over 48 hours
- Severe pain or high fever
- Persistent infections (3+ within six months)
Early intervention can help to avoid complications that come with eardrum perforation or mastoiditis (a rare but serious infection of the bones in the skull).
Treatment Options
Watchful Waiting
This isn’t true, and many mild infections do clear themselves. Antibiotics may not be prescribed until it has been monitored for 48-72 hours.
Medications
- Antibiotics (like amoxicillin) are used for infections by bacteria.
- Analgesics (ibuprofen or paracetamol) if pain is present.
Note: Overuse of antibiotics can help permit resistance, so they’re only prescribed when necessary.
Surgical Options
- Myringotomy (draining out fluid through a perforation).
- Surgical placement of ear tubes (also called tympanostomy tubes) in chronic cases may help ventilate the middle ear.
Preventing Ear Infections
1. Hygiene & Health Measures
- Frequent washing of your hands mitigates infection.
- Avoiding secondhand smoke lowers risk and irritation.
2. Vaccinations
- The most common bacterial agents are protected against by the pneumococcal vaccine (PCV).
- The risk of subsequent ear infections is decreased by annual flu vaccinations.
3. Feeding Practices
- Breastfeeding for up to six months increases resistance.
- Avoiding bottle-feeding babies could help reduce fluid accumulation.
Chronic Otitis Media: A Closer Look
Untreated chronic infections can lead to:
- Loss of hearing (children can have impaired speech development).
- Perforation in the eardrum or the presence of cholesteatoma (abnormal growth of skin).
Management includes:
- Regular ENT check-ups.
- Hearing tests if fluid is still present at age 3 months.
- Surgery to repair damage to his eardrums was a possibility.
When to Seek Specialist Care
See an ENT (ear, nose, and throat) specialist if you have:
✔ Chronic discharge from or pain in the ear
✔ Fever above 39°C
✔ Sudden hearing loss or lightheadedness
Conclusion
Ear infections are very common, but they’re something that should never be left untreated, especially if you are one of the children. Early recognition of symptoms and prompt care can prevent complications and support a quick recuperation. If you or your child has been troubled by long-term issues with your ears, Chase Lodge Hospital can offer specialist advice and treatment, including for ENT.
Need further advice or an appointment? Contact us today for comprehensive ear care.