Ear Canal Infections (Otitis Externa): Symptoms, Causes & Treatment
Ear Canal is a condition that affects the outer ear and coating of the eardrum known as Otitis Externa. Swimmer’s ear is commonly known as: An infection, caused by moisture, bacteria or fungus, that invades the tender skin of the ear canal. Whether you swim a lot, use earbuds often or have sensitive skin, knowing the signs and how to treat it can help avoid complications.
In this guide, we’ll look at the causes, symptoms and successful ways to treat Otitis Externa, plus what you need to do to prevent it from happening and keep your ears in good shape.
What is Otitis Externa?
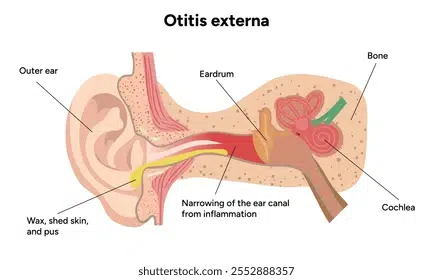
Otitis Externa is an infection or inflammation of the ear canal, which is a tube that runs from the outer ear to the eardrum. Otitis Externa is unrelated to Otitis Media (a middle ear disease, typically seen in children); instead, the external ear is infected, generally due to being exposed to water, being physically irritated, or having skin problems.
Acute vs Chronic Otitis Externa
- Acute Otitis Externa – It is a sudden, brief infection, which causes pain, redness and swelling. Usually caused by infections and clears with treatment in a few days.
- Chronic Otitis Externa — A long-term or recurrent infection lasting several weeks to months, usually because of underlying skin problems, such as eczema, or repetitive exposure to irritants.
Causes and Risk Factors
Ear canal infections may be caused by a number of things:
1. Trapped Moisture
The skin lining the ear canal is softened by prolonged exposure to water from swimming, showering, or a humid climate, which can create an environment with increased susceptibility to bacterial (and less commonly, fungal) infection. That’s why your head starts to itch when you’re in the water for too long. This is also partly why anyone who swims regularly is prone to “swimmer’s ear”.
2. Physical Injury or Irritation
- Putting cotton swabs, earbuds or fingernails in the ear, which can scratch the ear canal and let in bacteria.
- Moisture can be trapped or the ears rubbed by hearing aids or earplugs, leading to a higher risk of infection.
3. Skin Conditions and Allergies
- Eczema, psoriasis or seborrhoeic dermatitis can make the skin in the ear canal dry and flaky, which can mean it cracks and becomes infected.
- Hypersensitivity to hairsprays, shampoos, or earrings can also incite the inflammation.
4. Fungal and Bacterial Overgrowth
- Bacterial (frequently Pseudomonas aeruginosa or Staphylococcus aureus) infections flourish in damp surroundings.
- Fungal infections (such as Aspergillus or Candida) can occur after extended antibiotic treatment or in tropical environments.
Symptoms of Ear Canal Infections
The sooner you can recognise these warning signs, the better:
Common Signs
- Pain in the ear, especially when it is pulled or the patient chews.
- Itching inside the ear canal.
- Redness and swelling (The ear feels blocked).
Additional Symptoms
- A draining of fluid or pus (sometimes foul-smelling).
- Temporary loss of hearing from swelling or blockage.
- A sensation of fullness or pressure in the ear.
The infection may spread if not treated, which may cause fever and severe pain or even cellulitis (a skin infection).
When to See a Doctor
Those with mild symptoms can recover with home care and should seek medical attention if you:
- Your symptoms become severe or do not improve over a few days.
- You have a fever, a lot of discharge, or excruciating discomfort.
- You have diabetes or a compromised immune system, as infection can be rapid.
Diagnosis
A doctor will typically:
- Use an otoscope to look for redness, oedema, or drainage in the ear.
- Palpate the ear lightly to determine if it is tender.
- Culture (if a swab can be taken) to detect bacterial or fungal aetiological agents, particularly in repeat episodes.
Treatment Options
Otic and Topical Agents
- Antibiotic ear drops (such as ofloxacin or neomycin) for bacterial infections.
- Antifungal drops (for example, clotrimazole) if it is a fungus causing it.
- Steroid ear drops (such as hydrocortisone) to help decrease inflammation and itching.
Pain Relief
- Paracetamol/ibuprofen (over-the-counter pain relief medicine).
- Warm, wet compresses to relieve discomfort.
Professional Ear Cleaning
- A doctor can clear the debris or pus so the ear drops can work efficiently.
Severe or Chronic Cases
- If the infection spreads, use oral antibiotics.
- Consult an ENT specialist if the infection is not improving or is complex.
Self-Care and Home Remedies
What You Can Do
- Keep ears dry (use a low heat on a hairdryer if you have been swimming).
- Use OTC acetic acid drops, if prescribed.
What to Avoid
- Putting things (cotton swabs, fingers) in your ear.
- Applying (hydrogen peroxide, olive oil) home products without consulting a doctor.
Prevention Tips
After Swimming or Bathing
- Tip your head to let the water out.
- Wear swimmer’s earplugs if you have an infection proclivity.
Safe Ear Hygiene
- Don’t delve too deep into your ears; just use a moist towel to clean the outside.
- Continue to use alcohol-based drying drops for ear drying after water contact (if advised).
Managing Skin Conditions
- Use prescribed creams to manage eczema or allergies.
- Opt for hypoallergenic hair products if you’re sensitive.
Conclusion
Otitis Externa, although painful, is readily treatable with early attention. By spotting initial signs and avoiding triggers, you can stop infections from getting worse. If you have ongoing ear pain or discharge, we can help with experienced ear, nose and throat (ENT) specialists at Chase Lodge Hospital to diagnose and treat you.
Make an appointment today and receive professional ear care and peace of mind.