Understanding Crohn’s Disease: Symptoms, Diagnosis & Management
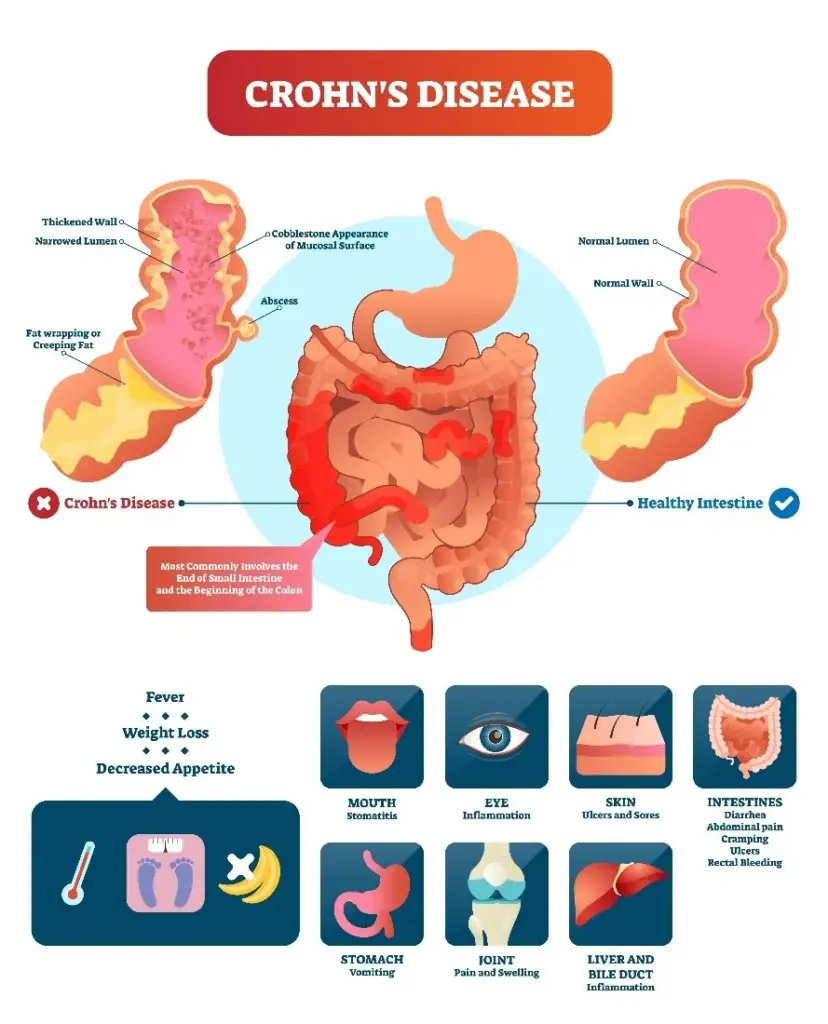 Image Source: colorectaldoc.com
Image Source: colorectaldoc.com
Crohn’s disease is an inflammatory disease that affects the digestive system, causing pain and discomfort, as well as debilitating symptoms. Unlike occasional stomach bugs, Crohn’s is a chronic condition which requires careful treatment to be able to continue living life to the fullest. We know the difficulties that people with Crohn’s can face and we offer expert care and support.
In this post, we’ll introduce Crohn’s disease: what it is, its symptoms and causes, and how you can identify it. We will also look at how to best manage the condition – be it through medical intervention or lifestyle changes – and how these can help you or a loved one cope better with the condition.
What is Crohn’s Disease?
Crohn’s disease is a type of inflammatory bowel disease (IBD) that causes chronic inflammation in the digestive tract. While it can affect any part of the gastrointestinal (GI) system—from the mouth to the anus—it most commonly impacts the ileum (the end of the small intestine) and the colon.
How is Crohn’s Different from Other IBDs?
Ulcerative colitis (UC), another type of IBD, is often mistaken for Crohn’s. But there are differences:
- The colon and rectum are the only areas affected by ulcerative colitis, which causes chronic inflammation.
- Crohn’s disease can involve any part of the GI tract, commonly as discrete, patchy areas involving distal or involved segments and can extend through the GI tract wall.
This distinction is critical for diagnosis and treatment.
Causes and Risk Factors
Although the precise causation of Crohn’s disease is uncertain, a number of variables are thought to be involved:
- Genetics: Family history of Crohn’s is a risk factor.
- Immune System Dysfunction: The immune system may receive inappropriate signals, encouraging it to begin attacking healthy bacteria in the gut.
- Environmental Triggers: Foods, smoking, and stress can make symptoms worse.
Who is at Risk?
- Age: Teens to people in their late 30s are most frequently diagnosed, but it can happen at any age.
- Family history: It’s more common if someone in the family has Crohn’s.
- Geography: More common in Western countries, perhaps linked to diet and lifestyle.
Common Symptoms
The symptoms of Crohn’s can vary from mild to severe and often come and go (flares and remissions).
Gastrointestinal Symptoms
- Diarrhoea that is usually (but not necessarily) bloody
- Cramp and/or pain in the abdomen (may be on the lower right side)
- Urgent bowel movements
- Mouth ulcers
Systemic Symptoms
- Unexpected loss of weight (poor absorption of nutrients)
- Tired feeling (from inflammation and anaemia)
- Joint pain and fever (during flares)
If you get these symptoms regularly, it’s important to see your GP.
Diagnosis of Crohn’s Disease
Crohn’s is diagnosed by means of a combination of symptoms and a process of exclusion.
Diagnostic Process:
- Patient History & Symptom Tracker – Review of symptoms and family history.
- Blood Tests – Looking for anaemia and markers of inflammation.
- Stool Tests – Testing for infections such as C. diff.
- Endoscopy/Colonoscopy – A camera is passed down the bowel and biopsies are taken.
- Imaging (MRI/CT scans) – Lesions can be found when looking for signs of inflammation, strictures, or fistulas.
Early diagnosis is the key to preventing complications, such as bowel obstructions or malnutrition.
Managing Crohn’s Disease
Despite the lack of a cure, a variety of therapies can help manage symptoms and enhance quality of life.
Medical Treatments
- Anti-inflammatory medication (such as corticosteroids) – To decrease acute inflammation.
- Immunosuppressive agents (for example, azathioprine) – To stop the immune system attacking.
- Biologics (e.g., anti-TNF therapy) – Targeted to specific inflammation pathways.
- Antibiotics – Used to treat infections such as abscesses.
Lifestyle & Diet Changes
- Find out what foods trigger an upset (common problem-makers: dairy, spicy food, high-fibre food).
- During flares, eat low-residue foods to facilitate digestion.
- Consume plenty of fluids to prevent dehydration while experiencing diarrhoea.
Surgical Options
If medications do not work or you have complications, you may need surgery, including:
- Strictures (narrowed portions of the bowel).
- Fistulae (abnormal connections between organs).
Procedures such as resection (cutting out damaged bowel) or strictureplasty (widening narrowed sections) can offer relief.
Living with Crohn’s: Coping and Support
Living with a chronic illness such as Crohn’s can be difficult but there is help.
Psychological Well-being
- Fatigue and social isolation are common — joining a support group can be a great idea.
- Counselling or therapy can help with stress and anxiety.
Tracking Symptoms
- Record flare-ups and triggers in a health journal.
- Periodic follow-up with a gastroenterologist allows for optimal care.
Prognosis and Outlook
Crohn’s disease is a chronic illness, yet with proper care:
- Many have long remission periods.
- New therapies, including biologics, and personalised care have brought hope.
- Trials are ongoing to identify better treatments.
When to Seek Help
Consult a specialist if you suffer from any of the following:
- Severe or long-lasting stomach pain
- Chronic diarrhoea or blood in the stool
- Unexplained weight loss
Early recognition is important to avoid complications and long-term effects.
Conclusion
Crohn’s disease is a complex disease, but one that can be managed. With timely diagnosis, successful treatment and lifestyle modification, most patients enjoy full and active lives.
If you think you may have Crohn’s disease or require specialist treatment, Chase Lodge Hospital is here to assist.
Make an appointment with our top-notch team of experts right now to start along the path to improved digestive health!
For more information, check out reliable sources such as Crohn’s & Colitis UK or the NHS website.