Why Am I Blood While Coughing? Haemoptysis Causes
& Medical Advice

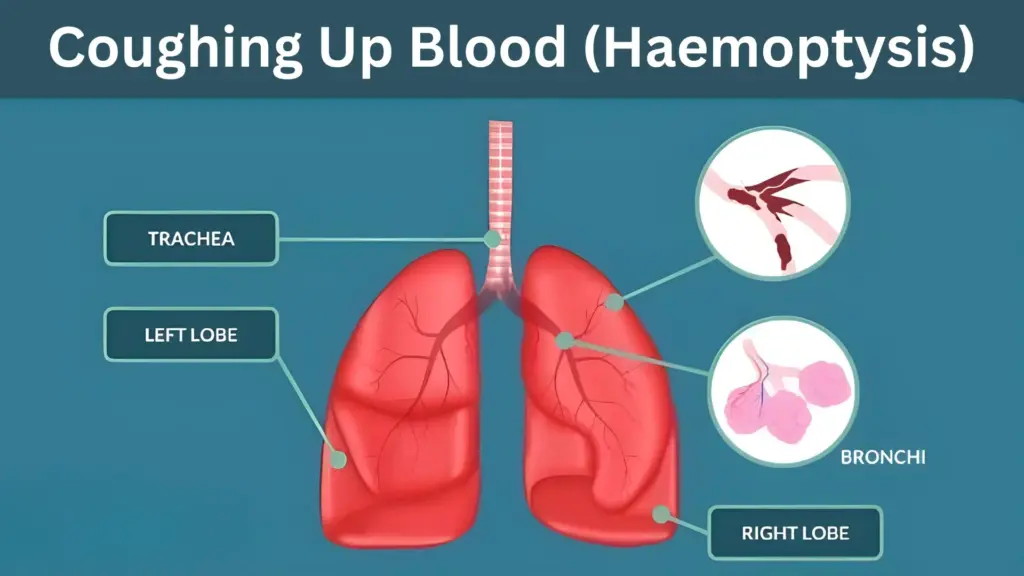
Blood during coughing, medically known as haemoptysis, can be a frightening experience. It refers to the act of blood comes out while coughing that originates from the lungs or airways. While it may sometimes be a minor issue, such as a burst blood vessel due to excessive coughing, it can also signal a more serious underlying condition. For individuals, understanding the causes for spitting blood treatment is crucial to ensuring timely and effective medical care.
What is Haemoptysis?
Haemoptysis is the term used to describe blood while coughing from the respiratory tract. This blood can appear as streaks in mucus or as larger amounts of pure blood. It’s important to distinguish haemoptysis from other conditions, such as vomiting blood (which originates from the stomach) or bleeding from the mouth or throat. True haemoptysis indicates a problem within the lungs or airways, and its severity can vary from mild to life-threatening.
Causes of Spitting up Blood
There are several potential causes for spitting blood, ranging from infections to chronic conditions. Some of the most common causes include:
- Bronchitis: Acute or chronic inflammation of the bronchial tubes can lead to irritation and bleeding. This is one of the more spitting blood causes.
- Pneumonia: A lung infection caused by bacteria, viruses, or fungi can result in inflammation and bleeding in the lung tissue.
- Tuberculosis (TB): Although less common in the UK today, TB remains one of the significant causes of haemoptysis worldwide. This bacterial infection primarily affects the lungs .
- Lung Cancer: Tumours in the lungs can erode blood vessels, leading to bleeding. Lung cancer is a serious condition that requires immediate medical attention.
- Pulmonary Embolism: A blood clot in the lungs can block blood flow, causing damage to lung tissue and resulting in haemoptysis. This is a medical emergency.
- Pulmonary Hypertension: High blood pressure in the arteries of the lungs can strain blood vessels, leading to bleeding.
Other less common causes of spitting up blood include bronchiectasis (a chronic lung condition), cystic fibrosis, and autoimmune diseases like lupus.
Symptoms Associated with Haemoptysis or Blood During Coughing
What causes blood in cough is often accompanied by other symptoms, which can help identify the underlying cause. These symptoms may include:
- Chest pain or discomfort, especially when coughing or breathing deeply.
- Shortness of breath or difficulty breathing.
- Fatigue or weakness, which may indicate a chronic condition or infection.
- Fever or night sweats, often associated with infections like pneumonia or TB.
- Weight loss, which can be a sign of a more serious condition like lung cancer.
If you experience any of these symptoms, it’s essential to seek medical advice promptly.
Blood During Coughing – Treatment for Haemoptysis
When you visit a healthcare professional for haemoptysis, they will begin by taking a detailed medical history and conducting a physical examination. To determine the underlying cause, they may recommend one or more of the following tests:
- Chest X-ray: This is often the first step to check for abnormalities in the lungs, such as infections or tumours.
- CT Scan: A more detailed imaging test that provides a clearer picture of the lungs and airways.
- Bronchoscopy: A procedure where a thin, flexible tube with a camera is inserted into the airways to look for sources of bleeding.
- Blood Tests: These can help identify infections or other systemic conditions.
- Sputum Analysis: Examining a sample of mucus can help detect infections like TB.
In some cases, additional tests such as pulmonary angiography (to check for blood clots) or a biopsy (to test for cancer) may be required. At Chase Lodge Hospital, we offer state-of-the-art diagnostic services to ensure accurate and timely results.
Treatment Options for Blood While Coughing
The treatment for haemoptysis depends entirely on the underlying cause. Here are some common approaches:
- Infections: If the cause is an infection like bronchitis, pneumonia, or TB, antibiotics, antivirals, or antifungal medications will be prescribed.
- Lung Cancer: Treatment may involve surgery to remove tumours, chemotherapy, or radiation therapy.
- Pulmonary Embolism: Blood thinners are often used to dissolve clots and prevent new ones from forming.
- Pulmonary Hypertension: Medications to lower blood pressure in the lungs may be prescribed.
- Severe Bleeding: In cases of significant haemoptysis, emergency interventions such as bronchial artery embolisation (to stop bleeding) or surgery may be necessary.
When to Seek Medical Help to Treat Causes for Spitting Blood
This problem should never be ignored, even if the amount of blood in cough seems small. While it may not always indicate a serious condition, it’s better to err on the side of caution. Seek immediate medical attention if:
- You cough up more than a few teaspoons of blood.
- You experience chest pain, shortness of breath, or dizziness.
- The bleeding persists or worsens over time.
Early spitting blood causes treatment can significantly improve outcomes, especially for serious conditions like lung cancer or pulmonary embolism.
Conclusion
Blood while coughing, or haemoptysis, is a symptom that warrants careful attention. While it can be caused by relatively minor conditions like bronchitis, it may also indicate more serious issues such as lung cancer or pulmonary embolism. Understanding the potential causes, recognising accompanying symptoms, and seeking prompt medical care are essential steps in managing this condition.
If you or someone you know is experiencing blood during coughing, don’t delay—book an appointment with a healthcare professional today.
References
- NHS. “Coughing up blood (haemoptysis).” Available at: https://www.nhs.uk/conditions/coughing-up-blood/.