
Understanding Cholecystitis: Symptoms, Causes, and Treatment Options
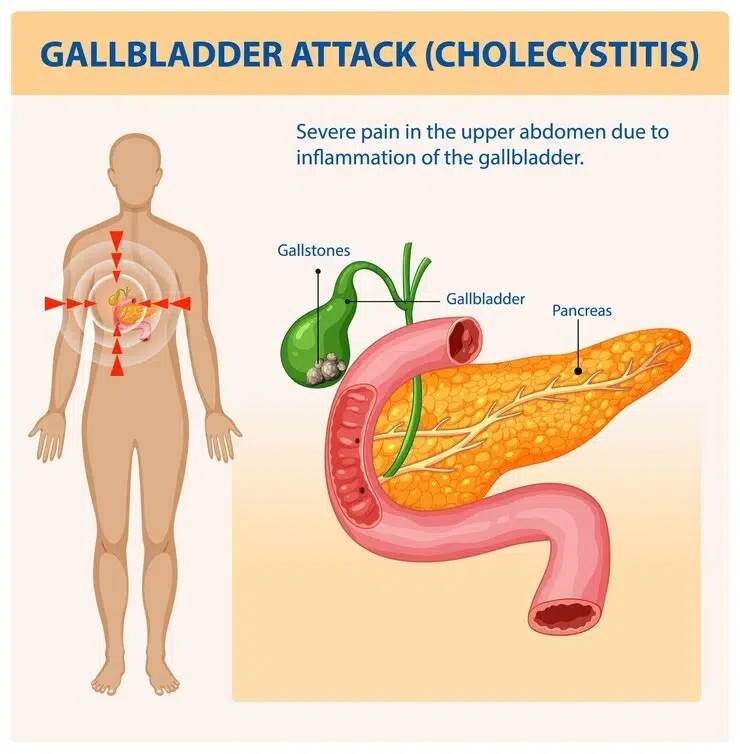
Cholecystitis is a medical problem marked by the inflammation of the gallbladder: a tiny organ lying below the liver storing bile, a digestive fluid required for the breaking of fats down to simpler forms. Both acute (sudden) and chronic (long-term) cholecystitis typically comes up, precipitated frequently by gallstones that obstruct the bile duct. In the absence of treatment, such conditions can result in severe complications, including gangrenous cholecystitis (tissue death) or empyema (pus-filled gallbladder), hence it is important to be diagnosed and treated early.
We offer specialised care for gallbladder-related conditions at the Chase Lodge Hospital, including cutting-edge robotic-assisted surgery for precision treatment. This blog will delve into the causes, symptoms, diagnosis, and treatment options available for an in-depth understanding of how to recognise these conditions and seek help.
What Causes Cholecystitis?
The most common factor that lays down the case of cholecystitis is gallstones, obstructing the cystic duct. They inhibit the flow of bile, permitting bile to build up, flood, and become inflamed or infected. Other causes are:
- Bile duct blockages – Tumours, scarring, or enlarged lymph nodes may compress the ducts.
- Infections – Inflammatory reactions in the bile are induced by bacterial infections, including rare parasites like liver flukes in endemic regions.
- Chronic gallbladder disease – Once inflamed over a number of episodes, the gallbladder may sustain damage, leading to porcelain gallbladder (calcification).
- Vascular problems – Impaired blood flow to the gallbladder could lead to tissue damage (e.g., in critically ill patients or vasculitis sufferers).
Certain predispositions are more likely to lead to cholecystitis, such as obesity, a high-fat diet, abrupt weight loss (e.g., post-bariatric surgery), diabetes, and being female, for women (for females are more prone to gallstones).
Recognising the Symptoms of Cholecystitis
The fundamental symptom is severe lumbar abdominal pain that is centred on the right side of the upper abdomen. The pain can become very excruciating down the back area or to the right shoulder; at times, the pain worsens after the consumption of fatty foods. Other symptoms include:
- Nausea and vomiting (may mimic food poisoning initially)
- Fever and chills (indicating infection, possibly sepsis if severe)
- Jaundice (yellowing of the skin and eyes due to bile blockage, suggesting choledocholithiasis)
- Bloating and indigestion (from impaired fat digestion)
- Loss of appetite (a red flag if prolonged)
Acute cholecystitis will often come with quite severe and intense pain, whereas for chronic cholecystitis, it can be milder and recurrent. Should you experience persistent pain in your abdomen along with fever, or jaundice, you must see a doctor right away, as this may be indicative of a substantial complication like gallbladder perforation.
How Is Cholecystitis Diagnosed?
The specialists at Chase Lodge Hospital use a wide range of advance diagnostic methods in order to affirm the diagnosis of cholecystitis. Here follows a general diagnostic procedure:
- Physical Examination – For abdominal tenderness assessment. (Murphy’s sign—pain on inspiration during palpation—is classic).
- Blood Tests – Elevated white blood cells indicate infection, whereas abnormal liver enzymes can be suggestive of bile duct obstruction (elevated ALP/GGT).
- Imaging Scans –
- Ultrasound – The most common test detecting the presence of gallstones and/or if there has been swelling in the gallbladder.
- CT or MRI Scan – If complications (e.g., abscesses or Mirizzi syndrome) are suspected, in that case, these scans may prove helpful in offering more detailed imagings.
- HIDA Scan – To monitor the flow of bile for the functioning of the gallbladder (EF <35% suggests chronic dysfunction).
An accurate diagnosis is to be established for the proper management that would in turn help in precluding anymore troublesome possible complications.
Effective Treatment Options for Cholecystitis
- Immediate Medical Management
- Hospitalisation – Severe cases may require IV fluids, antibiotics (e.g., piperacillin-tazobactam), and analgesics.
- Fasting – With food intake stopped, the gallbladder will not be active, temporarily putting it to rest.
- Surgical Treatment (Cholecystectomy)
Surgical removal of the gallbladder (cholecystectomy) is the only curative treatment for chronic or severe cholecystitis. At Chase Lodge, we offer:- Laparoscopic Cholecystectomy – A minimally invasive procedure, which is done through small incisions and allows for quicker recovery and rarely causes scarring.
- Open Surgery – It is used in more complex cases where it is not possible to do keyhole surgery (e.g., severe adhesions or fistulas).
- Most of the patients recover completely in a few weeks and are able to live a normally healthful life without a gallbladder. For bile flow from the liver to the intestines, no gallbladder is required anymore.
- Non-Surgical Alternatives
For patients unfit for surgery, alternatives include:- ERCP (Endoscopic Retrograde Cholangiopancreatography) – Removes bile duct stones (can be combined with sphincterotomy).
- Percutaneous Drainage – Drains infected fluid in high-risk patients (e.g., cholecystostomy tube placement).
Potential Complications of Untreated Cholecystitis
Disregarding symptoms may eventually lead to more serious complications, such as:
- Gangrene – Tissue death due to restricted blood flow (risk of Clostridial infection).
- Gallbladder Rupture – A surgical emergency leading to peritonitis (an abdominal infection).
- Chronic Pain & Digestive Issues – Long-term inflammation causing a state of severe illness and impaired absorption (e.g., fat-soluble vitamin deficiency).
Early intervention significantly reduces these risks.
Prevention and When to Seek Help
While not all cases are preventable, you can lower your risk by:
✔ Maintaining a healthy weight (BMI <30)
✔ Eating a balanced, low-fat diet (Mediterranean diet is protective)
✔ Avoiding rapid weight loss (>1.5kg/week increases gallstone risk)
✔ Managing underlying conditions (e.g., diabetes or metabolic syndrome)
Seek urgent medical advice if you experience:
- Sudden, severe abdominal pain (especially if radiating to the back)
- High fever with chills (>38.5°C suggests systemic infection)
- Jaundice (yellow skin/eyes with dark urine)
Conclusion:
While cholecystitis is indeed a severe condition, it is curable. Early diagnosis of its symptoms and seeking treatment from experts prevent complications and guarantee fast recovery. The team at the Chase Lodge Hospital is specialised in the diagnosis and treatment of all gall bladder conditions by means of the most up-to-date surgical, and non-surgical techniques, including single-incision laparoscopic surgery (SILS) for improved cosmesis.
If you suspect that you are carrying a cholecystitis infection, then book yourself an appointment with people that specialise in this matter and get specialised care.
For more information, visit:
NHS – Acute Cholecystitis