Bleeding in the Brain: Causes, Symptoms, and Treatment Explained
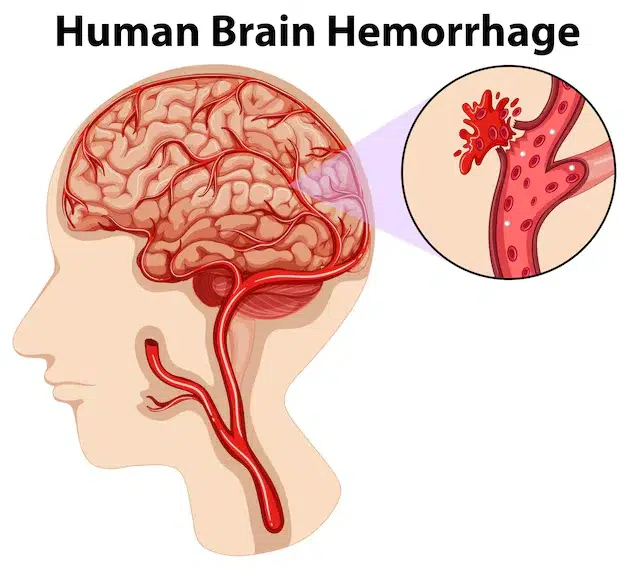
A cerebral bleed, also known as a brain bleed, occurs when a blood vessel ruptures, preventing the brain from functioning normally. This rapid-onset bleeding can create pressure on the brain, which can lead to serious complications or death if not treated quickly.
Whether resulting from high blood pressure, a blow to the head or an existing condition, spotting the symptoms early can be the difference between a full recovery and catastrophic outcomes. In this blog, we explain the different types, causes, signs and symptoms, and treatment options for brain haemorrhages, plus some key prevention measures to keep you healthy.
What is Bleeding in the Brain?
A brain haemorrhage occurs when a blood vessel bursts, causing bleeding within or around the brain. That bleeding starves brain cells of oxygen and raises pressure inside the skull, which can also damage brain tissue.
Strokes come in two main varieties: ischaemic (caused by a blocked artery) and haemorrhagic (caused by bleeding). They are also less common and more deadly, with haemorrhagic strokes accounting for around 15% of all strokes but producing a greater risk of severe disability or death.
Knowing the various types of brain haemorrhages enables the best approach to treatment.
Types of Brain Haemorrhage
1. Intracerebral Haemorrhage
- When a blood vessel in the brain bursts, blood spills into the surrounding tissue, causing that. It is closely associated with chronic hypertension, which over time can erode the arterial walls.
2. Subarachnoid Haemorrhage
- Bleeding occurs in the space between the brain and the thin membranes (meninges) that cover the brain. A ruptured aneurysm (a bulging blood vessel) is often the reason, resulting in a sudden and excruciating headache — it’s commonly referred to as the “worst headache of one’s life.”
3. Subdural Haemorrhage
- This type, which is usually the result of head trauma, is characterised by bleeding between the brain’s surface and its outer covering (dura). Patients on blood thinners and the elderly are more likely to experience it.
4. Epidural Haemorrhage (Not So Common)
- This is blood that accumulates between the dura and the skull, frequently as a result of a traumatic injury-induced skull fracture. It needs urgent surgical treatment.
Causes and Risk Factors
Some things can make you more likely to have a bleed on the brain:
1. Hypertension (High Blood Pressure)- The most common cause of intracerebral haemorrhage is high blood pressure, which weakens the walls of blood vessels over time.
2. Aneurysms- Blood vessels with weak spots that can rupture, often because of genetics or lifestyle risks such as smoking.
3. Head Trauma- Falls, car accidents and sports injuries can lead to bleeding, especially in children and the elderly.
4. Blood Disorders and Medications- Conditions such as haemophilia or the intake of blood thinners (e.g., warfarin) predispose to bleeding.
5. Brain Tumours- The tumours may cause the blood vessels to break, resulting in a haemorrhage.
Signs and Symptoms
Early recognition of symptoms can be life-saving. Look out for:
- Severe headache – It’s often restrictively described as a “thunderclap” headache.
- Nausea and vomiting
- Not understanding or speaking clearly
- Muscle weakness or numbness (particularly on one side of the body)
- Disturbances in vision (blurred or double vision)
- Seizures
- Loss of consciousness
If you or someone experiences these symptoms, call 999 immediately.
Diagnosis
Doctors may use the following diagnostic tools:
1. Physical & Neurological Examination
- Assesses alertness, coordination, and reflexes.
2. Imaging Tests
- CT scan – Early identification of bleeding.
- MRI – It shows clear and detailed images of the brain.
3. Additional Tests
- Blood tests (to test clotting function)
- Angiography (detects aneurysms or abnormal vessels)
Treatment Options
1. Emergency Management
- Preventing hyperventilation and lowering blood pressure
- ICU surveillance in patients with severe disease
2. Surgical Intervention
- Clot removal (craniotomy)
- Aneurysm clipping or coiling
3. Medications
- Blood pressure control
- Drugs which suppress swelling (such as corticosteroids)
- Anti-seizure medication
4. Rehabilitation
- Physiotherapy (brings back range of motion)
- Speech rehabilitation (helps with speaking)
- Cognitive therapy (memory and reasoning)
Prognosis and Recovery
Recovery depends on:
- Site and degree of haemorrhage
- Speed of treatment
- General health before the haemorrhage
Some will go on to make full recoveries; others may be left with severe long-term disabilities. Like any health problem, fighting eating disorders early is the best approach.
Prevention Tips
- Control blood pressure (regular monitoring)
- Prevent head injury (helmet, seatbelt use)
- Use blood thinners with care
- Quit smoking & limit alcohol
- Diet and exercise together
Conclusion
A brain haemorrhage is a life-threatening condition that needs urgent treatment. Understanding the symptoms, causes, and treatments can save lives. At Chase Lodge Hospital, we focus on fast diagnosis and specialist care to help improve your chances of recovery.
If you think it might be a brain haemorrhage, act quickly – seconds are precious. Keep up to date by visiting www.coronavirus.gov, take simple daily precautions, and use a tissue or your elbow to cover your nose and mouth ahead of an inevitable future meeting with a doctor.
For expert neurological care, contact Chase Lodge Hospital right now. Your health is our priority.